If you’re dealing with muscle pain or mobility issues, dry needling can help – but not all techniques are the same. Here’s a quick breakdown:
- Neurological Dry Needling: Targets nerve pathways to reduce pain and improve overall function. Ideal for chronic or widespread pain and neurological conditions.
- Trigger Point Dry Needling: Focuses on painful muscle knots (trigger points) to relieve localized pain and improve muscle performance. Best for acute, specific pain.
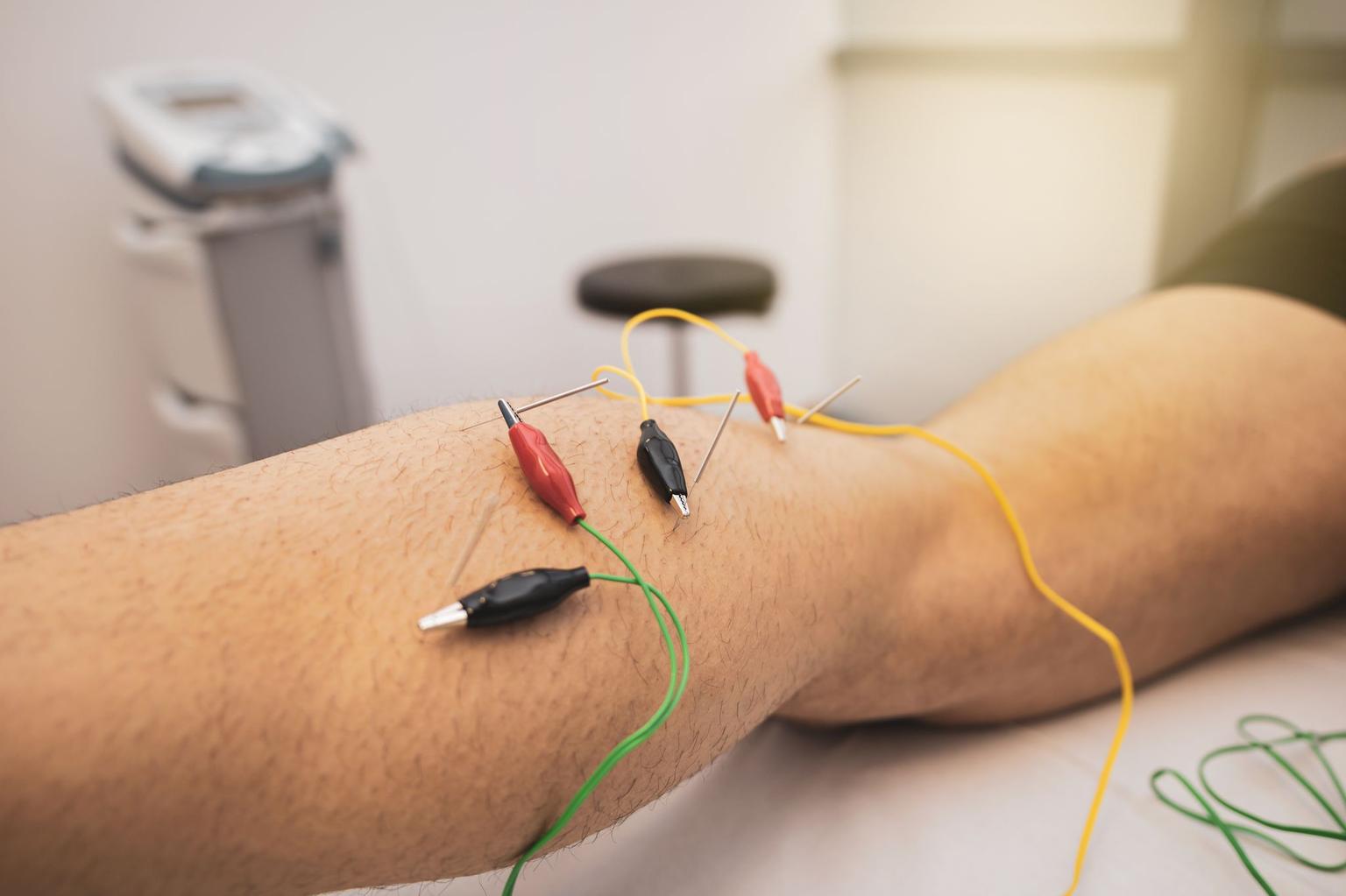
- Electrical Muscle Stimulation Dry Needling: Combines dry needling with electrical currents to enhance muscle activation and pain relief. Effective for chronic pain and conditions like sciatica or tendonitis.
Quick Comparison
| Technique | Primary Focus | Best For | Limitations |
|---|---|---|---|
| Neurological Dry Needling | Nerve pathways and systemic pain | Chronic pain, neurological issues | Requires advanced training |
| Trigger Point Dry Needling | Myofascial trigger points | Localized muscle pain | Limited to specific areas |
| Electrical Muscle Stimulation | Trigger points + electrical currents | Chronic pain, muscle activation | Needs specialized equipment |
Each method offers unique benefits, so consulting a trained professional is key to finding the right approach for your needs. Let’s dive deeper into how these techniques work and what to expect.
1. Neurological Dry Needling
Technique and Focus
Neurological Dry Needling takes a different approach compared to traditional dry needling methods by focusing on the nervous system instead of just targeting muscle knots. This technique involves placing needles near peripheral nerves, and in some cases, adding electrical stimulation to enhance nerve function. Unlike conventional methods that zero in on the pain site, this approach follows neurological pathways to influence pain signals at multiple levels, including local tissues, the spinal cord, and even the brain. By doing so, it taps into the body’s broader systemic responses, offering more than just localized relief [1][7][8].
Purpose and Benefits
The benefits of Neurological Dry Needling go beyond pain relief. It can improve flexibility, promote healing, reduce muscle tension, and even enhance athletic performance [10]. By addressing the neurological pathways responsible for pain and dysfunction, this technique helps reduce inflammation, increase blood flow, and ease muscle guarding [2]. Research also suggests that it can provide long-lasting relief for certain conditions, such as knee osteoarthritis, with pain reduction lasting up to four months for some patients [9].
Typical Clinical Uses
This method is versatile, making it useful for a wide range of neuromusculoskeletal conditions. It’s not just limited to orthopedic issues – it also addresses problems like neurogenic inflammation, poor blood flow, and muscle guarding [2]. Neurological Dry Needling has shown promise in treating nerve compression conditions like sciatica or pudendal neuralgia [1]. Additionally, it may positively influence the autonomic nervous system, potentially improving bowel and bladder function [1]. In cases of neurological disorders, the technique has been found to reduce spasticity, increase range of motion, and enhance voluntary movement, offering measurable improvements in function [11][12].
Patient Experience
For many patients, Neurological Dry Needling provides relief that extends beyond the immediate treatment area. Thanks to its focus on nerve pathways, improvements are often felt in related regions connected through the nervous system. The addition of electrical stimulation creates a unique sensation, delivering comprehensive relief that can be especially beneficial for those dealing with complex or chronic conditions. Patients frequently report a noticeable systemic effect, with benefits that reach beyond the primary pain site, making it a valuable option for addressing multifaceted issues.
2. Trigger Point Dry Needling
Technique and Focus
Trigger Point Dry Needling (TPDN) zeroes in on myofascial trigger points – those painful knots in muscles that can restrict movement and cause discomfort. This technique offers an option for patients whose pain stems from specific muscle knots, requiring a detailed understanding of anatomy. Using a thin needle, clinicians target these points by inserting the needle into the skin and muscle. A quick "pecking" motion creates tiny micro-injuries, which stimulate the body’s natural healing process. Often, this leads to a localized twitch response – a sign that the treatment is actively releasing muscle tension.
Purpose and Benefits
The main objective of TPDN is to break the cycle of pain caused by trigger points and help muscles function normally again. By addressing these active trigger points directly, the technique disrupts the chemical processes that sustain pain and helps reset the muscle tissue. Beyond pain relief, TPDN also promotes better blood flow and improves muscle performance. Many patients notice improvement after just one session, and studies back this up, showing enhanced range of motion and reduced musculoskeletal pain. This makes TPDN a valuable addition to comprehensive pain management plans that combine various therapies.
Typical Clinical Uses
Trigger Point Dry Needling is commonly used to treat joint problems, tendonitis, migraines, and TMJ disorders. It’s especially helpful for managing myofascial pain, chronic pain conditions, fibromyalgia, and tendinopathies. A 2017 study highlighted its effectiveness for lateral epicondylitis, showing that while it performed on par with NSAIDs, topical creams, ice, and braces at three months, it significantly outperformed them at six months [14]. Research has also revealed how quickly trigger points can develop – such as within 30 minutes of stressful computer use or just one hour of continuous typing in the upper trapezius muscle [13].
Patient Experience
During a TPDN session, clinicians carefully locate and palpate the trigger points to reproduce the patient’s pain symptoms. When the needle hits the right spot, it often triggers a brief muscle twitch – a hallmark of this technique. Dry needling is typically combined with other therapies, such as exercise, stretching, or massage, for a more holistic approach to pain relief. Adding proper stretching and strengthening exercises after treatment can enhance the results, offering targeted relief for persistent muscle knots that haven’t responded to other methods. This precise focus on localized pain prepares the ground for a balanced discussion of the technique’s pros and cons in the following section.
3. Electrical Muscle Stimulation Dry Needling
Technique and Focus
Electrical Muscle Stimulation Dry Needling (DNES) is a hybrid technique that combines trigger point dry needling with electrical stimulation. Thin stainless steel needles are inserted into trigger points – specific areas of muscle tightness – and a controlled biphasic electrical current is applied. This current helps relax tight muscle bands and induces controlled muscle contractions, which can aid in releasing tension. By merging these two methods, DNES enhances the effects of traditional dry needling, offering more targeted relief. The technique disrupts dysfunctional neuromuscular pathways, potentially speeding up the healing process. This allows physical therapists to address trigger points more effectively than using electrical stimulation alone [6][16].
Purpose and Benefits
DNES aims to relieve pain by targeting larger nerve fibers, which helps block pain signals and reduces the brain’s perception of discomfort [4][6]. Beyond pain relief, this technique improves blood circulation, increases muscle flexibility, reduces tension, and promotes the release of endorphins – natural chemicals in the central nervous system that act as painkillers [18]. Research has shown that combining dry needling with electrical stimulation can yield positive results for conditions like musculoskeletal shoulder pain, chronic low-back pain, and myofascial neck pain [6].
Typical Clinical Uses
DNES is particularly effective for managing myofascial pain syndrome, a condition affecting about one-third of individuals with chronic muscle pain [18]. It’s also used to treat a variety of conditions, including:
- Back, shoulder, and neck pain
- Carpal tunnel syndrome
- Lateral epicondylitis (tennis elbow)
- Plantar fasciitis
- Tendonitis
- Sciatica
- Headaches
Clinical studies highlight its effectiveness: patients undergoing DNES reported an average pain reduction of 4.8 ± 1.4 points, compared to 3.3 ± 2.2 points for those receiving conventional physical therapy. Disability scores also improved more significantly in DNES patients, with an average increase of 34.7 ± 9.1 points versus 20.1 ± 5.0 points for standard therapy [17]. This approach is particularly useful for targeting muscle groups like the upper trapezius, quadratus lumborum, and trapezius. Additionally, it can alleviate conditions like sciatica and carpal tunnel syndrome by reducing local muscle tension and improving blood flow [6].
Patient Experience
Patients undergoing DNES often describe sensations that set it apart from standard dry needling. When the electrical current is applied through the needles, they typically feel a mild tingling or tapping sensation as the muscle fibers contract and relax [6]. The intensity and duration of the stimulation are carefully tailored to each individual’s comfort and therapeutic needs. Clinicians closely monitor the patient’s response, ensuring the treatment remains comfortable while maximizing its benefits. These distinct sensations contribute to the enhanced therapeutic effects that make DNES a unique and effective approach compared to traditional dry needling methods.
sbb-itb-ed556b0
What Are The Types Of Dry Needling? How Electrical Stimulation Can Help
Benefits and Drawbacks
Each dry needling technique comes with its own set of strengths and limitations, shaping how and when it’s used. Here’s a closer look at the unique characteristics of these approaches and how they compare.
Neurological Dry Needling stands out for its ability to tackle complex pain patterns by targeting the nervous system through peripheral nerve mapping. This method goes beyond relieving localized pain – it helps reduce neurogenic inflammation and boosts microcirculation, offering broader benefits [19]. However, it requires advanced training, making it less accessible to practitioners who lack specialized education.
Trigger Point Dry Needling is more straightforward to learn and apply, focusing directly on specific muscle knots. It’s particularly effective for treating acute, localized pain where the source is easy to pinpoint. The hallmark muscle twitch response provides immediate feedback, confirming its effectiveness in reducing muscle tension and tone [4]. Its main drawback? A narrow focus that may miss broader neuromuscular issues.
Electrical Muscle Stimulation Dry Needling combines traditional dry needling with electrical stimulation to enhance pain relief. By stimulating larger nerve fibers, this approach helps block pain signals from smaller fibers [4]. While it offers amplified results, it requires specialized equipment and involves more intricate procedures, which may limit its accessibility.
When choosing a technique, clinicians can match the treatment to the patient’s specific needs. Despite differences, all three methods share common safety considerations. Minor side effects, such as bleeding (16.04%), bruising (7.71%), and pain during treatment (5.93%), occur in about 36.7% of cases, while serious adverse events are extremely rare, happening in fewer than 0.1% of treatments [20]. Research confirms that dry needling, when performed by trained professionals, is a safe option with very low risks of major complications [15].
The table below provides a quick comparison of the benefits, limitations, and ideal applications for each technique:
| Technique | Primary Benefits | Main Limitations | Best For |
|---|---|---|---|
| Neurological Dry Needling | Targets complex pain patterns; improves microcirculation | Requires advanced training; more complex to perform | Chronic, widespread pain; neurological conditions |
| Trigger Point Dry Needling | Delivers targeted relief with immediate feedback (muscle twitch) | Limited to localized points; may overlook broader dysfunctions | Acute, localized pain; specific muscle knots |
| Electrical Muscle Stimulation Dry Needling | Combines needling with electrical stimulation for enhanced relief | Needs specialized equipment; more complex procedures | Patients requiring enhanced stimulation |
Understanding these distinctions helps clinicians make informed treatment choices. Typically, sub-acute conditions respond well within two to three sessions, while chronic pain or trigger points may need five to six sessions [15]. Since patient responses and conditions vary, accurate diagnosis and customized treatment plans are key to achieving the best outcomes [15].
Conclusion
Understanding the distinctions between different dry needling techniques is key for both patients and practitioners in selecting the most effective treatment. Neurological Dry Needling works by adjusting nerve signals through specific pathways, while Trigger Point Dry Needling focuses on myofascial trigger points, often producing a local twitch response for direct relief. On the other hand, Electrical Muscle Stimulation Dry Needling combines traditional needling with electrical currents to further stimulate nerve fibers and manage pain effectively.
Choosing the right approach depends on several factors – practitioner expertise, the patient’s condition, and the specific pathology being treated. As Dr. JJ Thomas, DPT, MPT, CMTPT explains:
"Dry Needling is one of the most beneficial techniques we can utilize to shorten recovery time" [21].
However, the success of any dry needling technique relies heavily on the practitioner’s skill and knowledge.
"The effectiveness of dry needling depends on the therapist’s skill in accurately palpating myofascial trigger points and their knowledge of anatomical structures" [5].
Each technique requires different expertise. Neurological methods demand a deep understanding of nerve pathways, while trigger point techniques rely on precise palpation skills.
For patients exploring dry needling, consulting a qualified professional is essential. A skilled practitioner will assess your condition and recommend the most suitable approach, ensuring both safety and effectiveness. At Portland Chiropractic Group, our team combines evidence-based practices with personalized care to help you achieve your wellness goals.
Finally, dry needling works best when paired with complementary therapies like exercise and stretching [3]. By integrating these approaches into a personalized plan, practitioners can provide more effective and comprehensive care tailored to each individual’s needs.
FAQs
Which type of dry needling is best for my condition?
Choosing the right type of dry needling largely depends on your condition and what you hope to achieve from treatment. Here’s a quick breakdown of the main types:
- Trigger Point Dry Needling: This method targets those pesky, tight muscle knots that can cause localized pain. It’s especially useful for addressing acute muscle strains or areas of tension.
- Neurological Dry Needling: Designed to stimulate nerves, this approach is ideal for nerve-related issues like sciatica or nerve compression. It can help improve function and ease discomfort tied to these conditions.
- Electrical Muscle Stimulation Dry Needling: By combining traditional dry needling with electrical currents, this technique boosts blood flow, reduces inflammation, and supports recovery – making it a solid choice for more complex or chronic cases.
The best way to determine which method suits you is to consult with a qualified practitioner. They’ll evaluate your symptoms and guide you toward the most effective treatment plan to meet your wellness goals.
What are the potential risks or side effects of Neurological, Trigger Point, and Electrical Muscle Stimulation Dry Needling?
While dry needling techniques such as Neurological Dry Needling, Trigger Point Dry Needling, and Electrical Muscle Stimulation Dry Needling are considered safe when performed by qualified professionals, it’s important to understand the potential risks and side effects. The most common side effects include mild soreness, bruising, slight bleeding, or temporary fatigue following the procedure.
In rare cases, more serious risks can occur. These might include injury to nerves or blood vessels, and in extremely rare instances, complications like pneumothorax (a collapsed lung) if needles are improperly placed near sensitive areas. That said, such risks are uncommon, and for many, the benefits of dry needling outweigh these possibilities. To minimize risks and achieve the best outcomes, always choose a provider who is certified and has ample experience.
Can dry needling be used with other treatments to improve results?
Yes, dry needling works well alongside other treatments to improve results. When combined with approaches like physical therapy, manual therapy, or exercise programs, it can help ease pain, boost mobility, and speed up recovery. This makes it particularly useful for managing chronic pain, muscle tightness, or sports injuries.
By targeting muscle tension while addressing underlying issues, blending dry needling with other therapies doesn’t just relieve symptoms – it also promotes lasting recovery and functional progress. This combined approach allows for a more tailored and well-rounded plan for care.


Comments are closed