Welcome To Portland Chiropractic Group
At Portland Chiropractic Group we have created a warm and welcoming environment where patients feel comfortable and supported in their healthcare journey. Our state-of-the-art facilities and expert team enables us to provide the best possible evidence-based standard of care. We take the time to listen, understand, and tailor our approach to everyone’s needs, goals, and values. We empower patients with knowledge, tools, and support to take control of their health and well-being. Portland Chiropractic Group recognizes patient centered healthcare in its approach and we show up to work in order to witness you succeed in this endeavor. Our team is dedicated to delivering exceptional care with compassion, empathy, and kindness. Portland Chiropractic Group is a sanctuary for healing, where trust, confidentiality, and warmth foster a sense of safety, allowing you to explore, express, and transform true health and wellness. At Portland Chiropractic Group you’ll find a supportive community, free from judgment, where your autonomy and agency are respected and empowered. Together, we can co-create a tailored plan, blending the best of scientific insight with your values, goals, and lived experience, ensuring a truly personalized approach. Portland Chiropractic Group is dedicated to achieving the best available positive out-come for patients whether it is with Portland Chiropractic Group, another physician, or midlevel provider. We work for you, the patient, and will not budge from this platform. Portland Chiropractic Group upholds a commitment to providing care that is guided by the highest standards of ethics and compassion. Patients can expect to receive care that is patient-centered, respectful, and transparent, and that prioritizes their well-being and dignity.
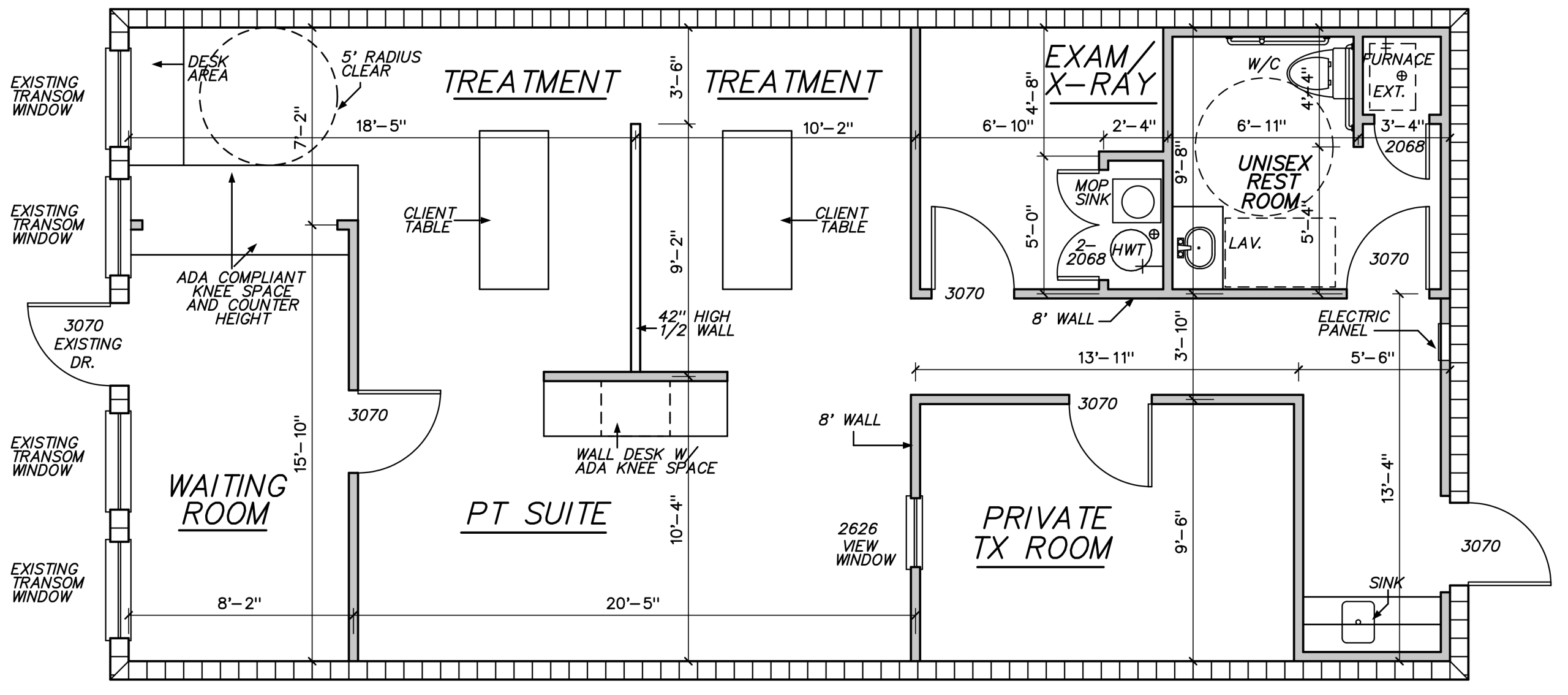
Open Floor Plans Promote Transparent Healthcare
At Portland Chiropractic Group we incorporate an open floor plan that is designed for the safety and security of all involved in your treatment. This includes the safety and security of patients that elect to participate in their healthcare journey with Portland Chiropractic Group. We have an open model to create transparency, accountability, and responsibility for our physicians and team members. Portland Chiropractic Group grants privacy regarding your medical health history, performance during examination procedures, and consultations about your diagnosis or diagnoses by providing a private area where we are able to explore these findings and ways to overcome them. Some procedures are done in an open environment, and if one is hesitant because of that, Portland Chiropractic Group will attempt to mitigate that hesitancy to see if we can provide you with the accommodations you are seeking.
Our Team

An Oklahoma native who was raised in Yukon where he mostly worked odd construction, maintenance, and landscaping jobs prior to and during his undergraduate career at the University of Central Oklahoma. He succumbed to low back pain during this period. Brett was suggested by a family member to seek a Chiropractic consultation with a trusted local physician after seeking alternatives to the over-the-counter products he was taking on a regular basis to get through the week. Having not had previous experience with Chiropractic and having been raised in a medical model of health, Brett was skeptical of Chiropractic. He attended the consultation because over the counter management just dulled his sharp pain, he was out of options, and his family member suggested it.
After the first visit, Brett was so impressed with the Chiropractor’s professional scope and ability to instantly relieve him of the sharp pain he felt upon sitting, that he decided to attend Parker Chiropractic College to become a chiropractor after extensive scrutiny in the UCO library. He currently serves the Oklahoma City community area with an evidenced-based passion for natural, non-pharmacological, and non-surgical approaches to acute and chronic pain conditions and syndromes.
Professional Interest
Functional Anatomy, General Biomechanics, Rehabilitation and Prevention, Therapeutic Exercise, Impingement Syndromes of the Shoulder, Discogenic Pain Syndromes, Cervicogenic Headaches, Pseudo and Spasmodic Torticollis, Glenohumeral Instability, Overuse Injuries, Chronic Pain Syndromes, Thoracic Outlet Syndrome, Whiplash Associated Disorders, Tendinopathies, Best Practice and Evidence Based Guidelines, Practice Parameters, Breathing Pattern Disorders, Functional Movement Patterns and Disorders, Inflammation and Pain Nutritional Considerations, Fascial Influence of Locomotion, Wellness and Preservation of Health, Effectiveness and Efficacy Trials of Low Back and Neck Pain, Management of Spine Disorders, Impairment and Disability Determination, Prognostic Factors for Low Back and Neck Pain
Frequently asked questions
We do not accept insurance. We chose not to accept insurance due to declining reimbursement rates, increased administration time, and to focus on specialized patient care. This allows us to set a fee schedule that
is similar in cost, if not lower, than your copay or coinsurance percentage. Most Americans do not meet their deductible each year, and most patients end up paying out-of-pocket for care. Insurance can be a great
investment for acute care situations that are unpredictable and high in cost (e.g., accidents, sudden illness, surgeries, traumatic injuries). The potential financial burden from a single acute event can reach tens
or hundreds of thousands of dollars. With acute care, insurance spreads risk among many people, making it affordable to cover rare, high-cost, events, and the premiums are manageable because most insured people
don’t experience catastrophic events each year.
Insurance is often less effective for chronic conditions, which are predictable and ongoing. Because insurers know these cost will recur, they price premiums and deductibles accordingly, often resulting in higher
annual costs. Chronic patients frequently encounter regular expenses that can quickly add up, hitting deductibles year after year. Patients often pay a substantial portion of chronic care cost out-of-pocket each
year, even with insurance. Cash or direct-pay alternatives (e.g., direct primary care or cash-pay pharmacies) often lower prices for routine chronic care services.
Insurance can be less advantageous financially for chronic disease care because you’re essentially paying premiums, deductibles, and coinsurance for predictable, unavoidable expenses. Cash-based models can be more
cost effective for chronic conditions, but insurance can still be beneficial if the chronic condition requires expensive specialty medications (e.g., biologics or cancer medications), frequent hospitalizations or
complications, or high-cost specialty care and or procedures. Even with chronic conditions, insurance can provide financial security and predictability by setting maximum annual out-of-pocket limits. However, for
routine, predictable chronic care (i.e., regular doctor visits, generic medications, and routine lab work), insurance often adds unnecessary overhead, leading to higher cost than cash-based options.
We proudly serve as an effective alternative to traditional clinics, bridging the gap between overpriced spinal health care and affordable, high-quality services. Our location is directly managed and operated by
chiropractic physicians, allowing us to streamline operations and significantly reduce administrative overhead and inefficiencies. By eliminating unnecessary bureaucracy, we can provide shorter, more cost-effective
procedures compared to traditional clinical settings. Administrative cost and insurance billing requires extensive administrative labor, coding, compliance, and appeals. Large health care facilities and hospitals
negotiate individually with each insurer, often leading to higher contracted rates compared to transparent cash-pay facilities. Hospital facilities and independent clinics have differing “place of service – POS”
codes for the location and setting the treatment was rendered.
For example, patients paying cash upfront at independent imaging facilities typically save 50-70% more compared to using insurance at hospitals or hospital-owned imaging centers. If you are insured and have not
met your deductible, one can typically pay an exorbitant amount for the diagnostic imaging. Even if you have met your deductible, and depending on the scenario, you will still most likely be paying more than the
cash market rate around Oklahoma City for diagnostic imaging (i.e., high coinsurance percentage, high allowed amount negotiated by insurance, and low cash prices offered by independent imaging centers).
We remain dedicated to transforming healthcare delivery, advocating for a patient-focused approach that ensures individuals receive essential spinal health care treatments and modalities without facing financial
hardship incurred by the fee schedule implemented from being in-network and not meeting your deductible. We have more freedom to bypass this fee schedule with the implementation of our own fee schedule, which translates
into lower cost for you, the patient. Not only does it decrease cost, but also physicians in cash-based models often experience higher job satisfaction due to fewer administrative burdens, reduced burnout, and greater
autonomy. Satisfied and less stressed clinicians typically provide better patient care resulting in higher quality patient outcomes.
Why cash-based clinics may obtain better patient health outcomes compared to insurance-based clinics:
Doctors of Chiropractic (DCs) care for patients of all ages, with a variety of health conditions. They are especially well known for their expertise in caring for patients with back pain, neck pain and headaches using their highly skilled manipulations or chiropractic adjustments. DCs also care for patients with a wide range of injuries and disorders of the neuromusculoskeletal system, which includes the nerves, muscles, ligaments and joints. These painful conditions may involve or impact the nervous system, which can cause referred pain and dysfunction distant to the region of injury. In addition, chiropractors offer advice to patients on diet, nutrition, exercise, healthy habits, and occupational and lifestyle modification.
Chiropractic is widely recognized as one of the safest nondrug, noninvasive forms of health care available for the treatment of neuromusculoskeletal complaints. Although chiropractic has an excellent safety record, no health treatment is completely free of potential adverse effects. The risks associated with chiropractic, however, are very small. Many patients feel immediate relief following chiropractic treatment, but some may experience mild soreness, stiffness or aching, just as they do after some forms of exercise. Current research shows that minor discomfort or soreness following spinal manipulation typically fades within 24 hours. Neck pain and some types of headaches are treated through precise cervical manipulation. Cervical manipulation, often called a neck adjustment, works to improve joint mobility in the neck, restoring range of motion and reducing muscle spasm, which helps relieve pressure and tension. Neck manipulation, when performed by a skilled and well educated professional such as a doctor of chiropractic, is a remarkably safe procedure. Some reports have associated high-velocity upper neck manipulation with a certain rare kind of stroke, or vertebral artery dissection. However, evidence suggests that this type of arterial injury often takes place spontaneously in patients who have pre-existing arterial disease. These dissections have been associated with everyday activities such as turning the head while driving, swimming, or having a shampoo in a hair salon. Patients with this condition may experience neck pain and headache that leads them to seek professional care at the office of a doctor of chiropractic or family physician, but that care is not the cause of the injury. The best evidence indicates that the incidence of stroke associated with high-velocity upper neck manipulation is extremely rare—about one in 1,000,000 patients who get treated with a course of care. This is similar to the incidence of this type of stroke among the general population. If you are visiting your doctor of chiropractic with upper-neck pain or headache, be very specific about your symptoms. This will help your doctor of chiropractic offer the safest and most effective treatment, even if it involves referral to another healthcare provider. When discussing the risks of any healthcare procedure, it is important to look at that risk in comparison to other treatments available for the same condition. In this regard, the risks of serious complications from spinal manipulation for conditions such as neck pain and headache compare very favorably with even the most conservative care options. For example, the risks associated with some of the most common treatments for musculoskeletal pain (i.e. over-the-counter or prescription nonsteroidal anti-inflammatory drugs (NSAIDS) and prescription painkillers) are significantly greater than those of chiropractic manipulation. Moreover, the Centers for Disease Control and Prevention (CDC) has reported that overuse and abuse of prescription opioid pain medications is among the leading causes of accidental death in the United States. Doctors of chiropractic are well trained professionals who provide patients with safe, effective care for a variety of common conditions. Their extensive education prepares them to identify patients who have special risk factors and to ensure those patients receive the most appropriate care, even if that requires referral to a medical specialist.
Doctors of chiropractic are educated as primary-contact portal of entry physicians, with an emphasis on diagnosis and treatment of conditions related to the neuromusculoskeletal system (the muscles, ligaments and joints of the spine and extremities) and the nerves that supply them. The typical applicant for chiropractic college has already acquired nearly four years of pre-medical undergraduate college education, including courses in biology, inorganic and organic chemistry, physics, psychology and related lab work. Once accepted into an accredited chiropractic college, the requirements become even more demanding — four to five academic years of professional study are the standard. Doctors of chiropractic are educated in orthopedics, neurology, physiology, human anatomy, clinical diagnosis including laboratory procedures, diagnostic imaging, exercise, nutrition rehabilitation and more. Because chiropractic care includes highly skilled manipulation and adjusting techniques, a significant portion of time is spent in clinical technique training to master these important manipulative procedures. In total, the chiropractic college curriculum includes a minimum of 4,200 hours of classroom, laboratory and clinical experience. The course of study is approved by the Council on Chiropractic Education, an accrediting agency that is recognized by the U.S. Department of Education.
Chiropractic adjustment, or manipulation (HVLA) is a hands on manual procedure that utilizes refined athletic skill developed during the chiropractors years of hands on training during their chiropractic education. The chiropractic physician
typically uses his or her hands or an instrument to adjust or mobilize the joints of the body, particularly the spine and extremities in order to restore or enhance joint function. Chiropractic adjustments are a highly controlled procedure
that rarely should cause discomfort, and if it does, let your chiropractor know. The chiropractor should adapt the procedure to meet the specific needs of each patient. Typically, the chiropractor will perform a quick thrust with his hands
in the plane line of the joint in an attempt to “cavitate” a joint. Cavitation is akin to the audible sound heard, joint movement felt, and increased range of motion found upon popping ones knuckles. Chiropractors have a strict adherence to
medical necessity. To identify a lesion worthy of adjusting requires 3 of 5 things: pain on palpation, asymmetry, range of motion restriction, tissue texture tone and temperature, and special test (radiological, neurological and or orthopedic
testing).
The length of treatment varies depending on the individual’s condition, severity, aggravation/re-aggravation of symptoms, and response to care. Some patients may experience relief after a few visits, while others may not. Your chiropractor will
develop a treatment plan tailored to your specific needs, and will discuss the expected duration of care with you depending on your goals, motivations, and financial availability. If you are not responding to care in 6-8 visits, then your
chiropractor will have a discussion with you regarding what other options exist for your condition.
The frequency of adjustments depends on your individual condition and the recommendations of your chiropractor. Initially, if warranted, you may need to be adjusted more frequently (e.g., several times per week) to address acute pain and inflammation.
As your condition improves, the frequency of adjustments may be reduced. Many people choose to continue with maintenance care to maintain their spinal health and prevent future problems. Most importantly, it is recommended to get motivated
and implement a long term exercise strategy that compliments your condition to prevent future problems and recurrence of symptoms. This enables independence from your chiropractor regarding how often you need to be adjusted.
Not necessarily. The goal of chiropractic care is to restore proper joint function, reduce pain, and promote healing. Once your condition has stabilized, you may choose to discontinue care or continue with maintenance care. Maintenance care can help prevent future problems and maintain optimal spinal health. The decision is ultimately up to you and your chiropractor’s recommendations. It is worth noting that once you have had back pain, a future likely occurence is higher than if you have never had back pain at all.
The traditional chiropractic philosophy, with its emphasis on “innate intelligence” and widespread “vertebral subluxations” causing systemic disease, lacks strong scientific support and can be considered pseudoscientific by many. Historically, the concept of “vertebral subluxation” was central to chiropractic. This was defined as a misalignment of vertebrae that interfered with nerve function and caused disease. This traditional view held that correcting these subluxations could improve overall health, even for conditions not related to the spine (e.g., hearing loss or organic disease). Modern nuanced approaches incorporate biomechanics and limit the amount of health disparities that can and do occur with restricted joint function. Many modern, evidence-based chiropractors use the term “segmental dysfunction” (or related terms like “joint dysfunction” or “joint restriction”) in a biomechanical sense, referring to joints that have limited range of motion or altered movement patterns. This is a different concept from the traditional, vitalistic definition, and this type of biomechanical dysfunction is supported by research and acknowledged by most everyone in the field of chiropractic.
The American Medical Association (AMA) also had a role in supplying this ideology to the public through underhanded professional ethics. See our latest blog post regrading “What Medicine Should Do About the Chiropractic Menace.”
Yes, chiropractic care is generally considered safe during pregnancy. In fact, it can be very beneficial for pregnant women, helping to alleviate back pain, sciatica, and other common pregnancy-related discomforts. Chiropractors are trained to use gentle techniques that are safe for both the mother and the baby. Some chiropractors have specialized training in prenatal chiropractic care.

