Diagnosing gluteal tendinopathy, a common cause of lateral hip pain, often relies on clinical tests. While MRI is accurate, it’s expensive, not always accessible, and sometimes shows abnormalities in symptom-free individuals. Clinical tests offer a practical alternative, but no single test is perfect. Here’s what you need to know:
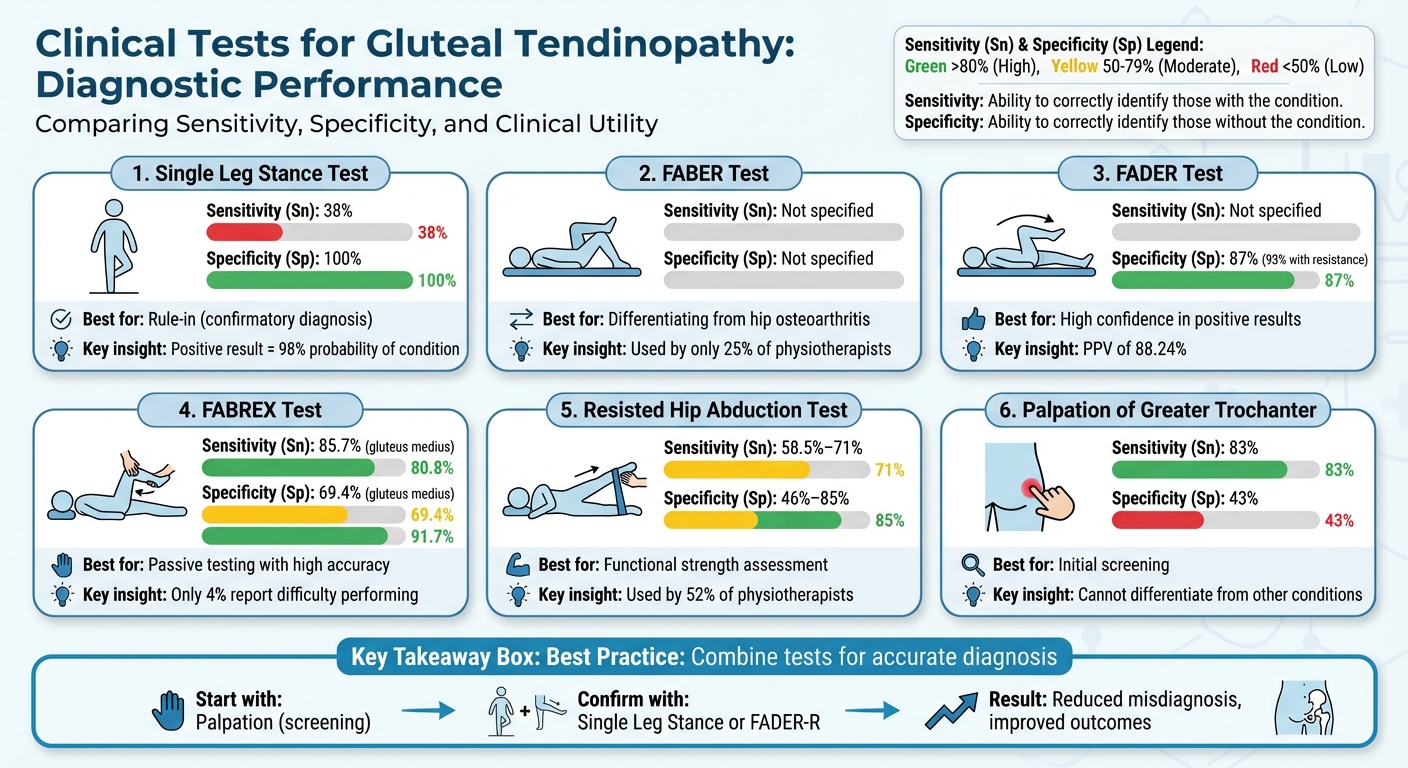
- Single Leg Stance Test: Highly specific (100%) but low sensitivity (38%). A positive result strongly confirms the condition.
- FABER Test: Useful for differentiating gluteal tendinopathy from hip osteoarthritis but lacks specific diagnostic data.
- FADER Test: Specificity of ~87%. Adding resistance (FADER-R) boosts accuracy to 93%.
- FABREX Test: High sensitivity (85.7%) and specificity (up to 91.7%). Promising but needs more research.
- Resisted Hip Abduction Test: Moderate sensitivity (58.5%-71%) and variable specificity (46%-85%). Best used with other methods.
- Palpation of Greater Trochanter: High sensitivity (83%) but low specificity (43%). Good for initial screening.
Quick takeaway:
For accurate diagnosis, combine tests. Start with palpation for screening, then use specific tests like the Single Leg Stance or FADER-R to confirm. This layered approach reduces misdiagnosis and improves patient outcomes.
Clinical Tests for Gluteal Tendinopathy: Sensitivity and Specificity Comparison
Key Clinical Tests for Diagnosing Gluteal Tendinopathy: Evidence-Based Guide
1. Single Leg Stance Test
The Single Leg Stance (SLS) test is a straightforward diagnostic tool used to identify potential lateral hip pain. During this test, the patient stands on the affected leg for 30 seconds while facing sideways to a wall for balance. The opposite leg is lifted with the knee bent at a 90-degree angle, keeping the hip in a neutral position. If the test triggers lateral hip pain within the 30-second timeframe, it’s considered a positive result [8].
Sensitivity
The SLS test has a sensitivity of 38% for detecting lateral hip pain [8]. This means it can miss many cases. For instance, in a study of 65 participants, 31 individuals with MRI-confirmed gluteal tendinopathy tested negative on the SLS [8]. Earlier research by Lequesne and colleagues reported a much higher sensitivity of 100%, but their study compared symptomatic patients to those with no pain, rather than to individuals with other causes of lateral hip pain [8][10].
Specificity
Where the SLS test truly stands out is in its specificity, which is an impressive 100% [8]. A positive result is almost always associated with MRI-confirmed gluteal tendinopathy, giving it a 100% positive predictive value [8]. If the test is positive, the likelihood of gluteal tendinopathy jumps from a baseline probability of 50% to 98%, thanks to a positive likelihood ratio of about 12 [8][6][9].
Clinical Utility
The SLS test is best suited as a rule-in tool. A positive result strongly confirms gluteal tendinopathy, making it valuable for distinguishing this condition from other causes of lateral hip pain [8]. However, a negative result doesn’t eliminate the possibility of gluteal tendinopathy, so it’s essential to use this test alongside other diagnostic methods as part of a comprehensive evaluation [1][3]. Clinicians can also use the test to monitor progress – less pain during the SLS can indicate improved tendon loading tolerance, showing how well the patient is responding to treatment [1].
Ease of Application
The SLS test is simple to perform and requires no special equipment beyond a wall for balance [3]. It takes just 30 seconds and fits seamlessly into any standard physical exam. Proper technique is critical, though – keeping the hip neutral and the knee at 90 degrees ensures accurate results [8]. This quick and accessible test sets the stage for comparing its effectiveness with other diagnostic tools. Up next: an analysis of the FABER test’s diagnostic role.
2. FABER Test
The FABER test involves positioning the hip in a figure-four shape. During the test, the patient lies on their back while the clinician places the affected leg in this configuration. If the patient experiences lateral hip pain during this process, the test is considered positive [1].
Clinical Utility
Although specific sensitivity and specificity data for identifying MRI-confirmed gluteal tendinopathy are not available, the FABER test is a valuable tool for differentiating between conditions. It is particularly helpful in distinguishing gluteal tendinopathy from hip osteoarthritis. For instance, patients who report lateral hip pain and tenderness over the greater trochanter during the FABER test but can still perform tasks like putting on shoes and socks without difficulty are more likely to have gluteal tendinopathy rather than hip osteoarthritis [1][3]. Even without exact diagnostic metrics, the FABER test plays a key role in identifying gluteal tendinopathy and ruling out other hip issues.
Ease of Application
Despite its usefulness, only about 25% of physiotherapists in Australia, New Zealand, Ireland, and the UK report using the FABER test in their practice [3]. Its ability to serve as a differential diagnostic tool highlights its importance, especially when compared to other testing methods.
3. FADER Test
The FADER test (Flexion, Adduction, and External Rotation) is performed by having the therapist passively move the patient’s leg into a position of 90° hip flexion, followed by adduction across the body and external rotation to its limit [1]. This movement causes the iliotibial band to shift over the greater trochanter, placing tension on the gluteus medius and gluteus minimus tendons. A test is considered positive if the patient reports a pain level of 2/10 or higher on the Numeric Rating Scale over the lateral hip [1].
Specificity
Studies show that the FADER test has a specificity of approximately 86.67% when compared to MRI imaging [7]. Adding static resisted internal rotation (known as the FADER-R test) boosts specificity to about 93.3% [11]. The test also has a positive predictive value of around 88.24%, meaning a positive result is strongly associated with gluteal tendinopathy [7].
Clinical Utility
Alison Grimaldi, PhD, a physiotherapy researcher at the University of Queensland, highlights the importance of active muscle contraction in diagnostic tests:
"Physical tests that involve an active muscle contraction component are most useful in identifying gluteal tendinopathy as diagnosed by MRI." [7]
While a positive FADER test is a reliable indicator of gluteal tendinopathy, it has a high false negative rate. To address this limitation, clinicians often combine it with more sensitive methods, like pinpoint palpation, to ensure no cases are overlooked and to enhance diagnostic accuracy. Up next, we’ll explore the FABREX test as another diagnostic tool.
4. FABREX Test
The FABREX test is a passive diagnostic technique used to identify gluteal tendinopathy. It works by relaxing the iliotibial complex while the clinician moves the patient’s hip through flexion, abduction, and external rotation. The key to this test is that the patient remains completely relaxed, minimizing the risk of misinterpretation.
This test demonstrates a high sensitivity – 85.7% for the gluteus medius and 80.8% for the gluteus minimus – making it reliable for ruling out the condition when the result is negative. Its specificity is also noteworthy, with 69.4% for the gluteus medius and 91.7% for the gluteus minimus, meaning a positive result strongly supports the diagnosis.
The FABREX test is straightforward to perform in clinical settings, with only 4% of patients reporting any difficulty. However, as this test is still in its early stages of validation, additional research is necessary to verify its consistency across different clinicians and patient groups [4]. These promising metrics suggest the FABREX test could become a valuable tool in diagnosing gluteal tendinopathy and warrant further comparisons with other diagnostic methods.
sbb-itb-ed556b0
5. Resisted Hip Abduction Test
The Resisted Hip Abduction Test is widely used by physical therapists, with 52% incorporating it into their clinical assessments for gluteal tendinopathy [3]. The test involves the patient actively moving their leg away from the body while the clinician applies resistance. The goal is to provoke pain in the hip abductor muscles, helping to identify potential issues [1]. This test is often compared to others to evaluate its sensitivity and specificity.
Sensitivity
Studies show the test has a moderate sensitivity, ranging from 58.5% to 71% [12][1]. In practical terms, this means it correctly identifies 58.5% to 71% of cases, leaving about 30–40% as false negatives.
Specificity
Specificity for the test varies widely, from 46% to 85%, depending on the study and the position used during the test [12][1]. A systematic review by Reiman et al. found a sensitivity of 71% and a specificity of 84% [1], indicating that a positive result can be fairly dependable when the test is performed correctly. Additionally, combining the test with palpation of the greater trochanter can significantly improve the likelihood of diagnosing greater trochanteric pain syndrome [13][14].
Clinical Utility
The test’s diagnostic value increases when patients are asked to pinpoint the exact location of their pain rather than just confirming its presence [12]. Performing the test with the hip in an adducted position can further enhance its diagnostic accuracy [1]. However, it’s important to note that resistance tests like this one are susceptible to variations in clinician technique [12]. For a more accurate diagnosis, this test should be used alongside other assessments [1].
Ease of Application
Resisted hip abduction is a fundamental skill taught during undergraduate physical therapy programs [3]. However, its reliability can be affected by the clinician’s level of experience [12]. Less experienced therapists often perform the test with the hip in a neutral position, which may impact results [3]. While the test is straightforward to administer, interpreting the findings accurately requires clinical expertise and should be part of a broader diagnostic approach [3].
6. Palpation of Greater Trochanter
Palpating the greater trochanter involves applying pressure to the bony prominence on the outer hip. This is done while the patient lies on their side with hips flexed at 60° and knees together. A positive result occurs when the patient reports pain or tenderness in the area [1].
Now, let’s break down its diagnostic performance, starting with sensitivity.
Sensitivity
The test shows a sensitivity of 83% [1], meaning it correctly identifies about 8 out of 10 patients with the condition. This makes it a valuable screening tool, especially in physiotherapy settings, where high sensitivity is crucial for identifying potential cases [3].
Specificity
The specificity, however, is much lower at 43% [1]. This indicates that more than half of the patients who show tenderness during palpation might not actually have gluteal tendinopathy. As Dr. Alison Grimaldi explains:
"Tenderness on palpation alone is not adequate for a diagnosis of gluteal tendinopathy/GTPS as many people are tender over the greater trochanter without necessarily having gluteal tendinopathy/GTPS (low specificity)." [3]
This low specificity highlights the test’s limitations when used in isolation, as it cannot reliably distinguish gluteal tendinopathy from other causes of hip pain.
Clinical Utility
While palpation is considered a key indicator of gluteal tendinopathy, it should never be used as the sole diagnostic method [1][3]. Its low specificity means it often fails to differentiate between gluteal tendinopathy and other lateral hip pain conditions. To enhance diagnostic accuracy, clinicians should combine palpation with other tests like the FADER test and Single Leg Stance test [1][3]. This multi-test approach minimizes misdiagnosis and ensures patients receive the right treatment.
Ease of Application
Palpation is a fundamental skill taught early in physiotherapy training [3]. It’s quick, requires no equipment, and is easy to perform, making it highly practical in busy clinical environments. Its simplicity and accessibility contribute to its widespread use. In fact, it’s one of the three most commonly used diagnostic tests, alongside the Single Leg Stance test and resisted hip abduction [3]. However, its widespread use underscores the importance of pairing it with more specific tests for a well-rounded diagnosis.
Advantages and Limitations of Each Test
Each diagnostic test comes with its own set of strengths and weaknesses, which is why clinicians often rely on a combination of methods to achieve a more accurate diagnosis. Here’s a summary of the key characteristics of these tests:
| Clinical Test | Sensitivity | Specificity | Best Used For | Key Limitation |
|---|---|---|---|---|
| Single Leg Stance Test | 38% | 100% | Confirmatory diagnosis when positive | Low sensitivity; a negative result doesn’t rule out the condition |
| FADER Test | Not specified | 86.67% | High confidence in positive results (PPV 88.24%) | Limited use in clinical practice |
| FABREX Test | High (gluteus medius) | High (gluteus minimus) | Simple, accurate passive testing | None noted |
| Resisted Hip Abduction Test | Varies | Varies | Functional strength assessment | Less specific than other tests |
| Palpation of Greater Trochanter | 83% | 43% | Initial screening | Cannot differentiate from other hip conditions |
Let’s break this down further. The Single Leg Stance Test stands out with a 100% positive predictive value, meaning a positive result is highly reliable. However, its low sensitivity means it might miss many cases, as a negative result doesn’t rule out the condition entirely [1]. On the other hand, palpation of the greater trochanter is highly sensitive but lacks specificity. This means that while it’s good for initial screening, tenderness detected through palpation might often be due to other hip conditions, not just gluteal tendinopathy [1].
Interestingly, specialized tests like the FADER-R and ADD-R are underused, with only about 35% and 38% of physiotherapists, respectively, incorporating them into practice [3]. This contrasts with the FABREX test, which is much easier to perform – only 4% of clinicians report difficulty using it, compared to 54% for the more cumbersome Lequesne test [4]. This ease of use makes the FABREX test particularly valuable in fast-paced clinical environments.
Relying on just two or three tests can increase the risk of misdiagnosis. A better approach combines a sensitive screening tool, like palpation, with a more specific test, such as the Single Leg Stance Test. Additionally, modifications like adding resisted isometric internal rotation to the FADER test can further improve diagnostic precision [11]. This comprehensive strategy ensures patients receive more accurate diagnoses and, ultimately, better care.
Conclusion
Diagnosing gluteal tendinopathy effectively requires using a combination of clinical tests rather than relying on a single method. For instance, when the Single Leg Stance test provokes pain within 30 seconds, the probability of MRI-confirmed gluteal tendinopathy jumps significantly – from 50% to 98% – but its low sensitivity means it often misses cases if used on its own[5][6][7][15][16].
A good starting point for screening is greater trochanter palpation, which has an 80% sensitivity rate. A negative result here can significantly reduce the likelihood of gluteal tendinopathy[5][6][7][15]. However, if tenderness is detected, more specific tests like the Single Leg Stance or active resistance methods should follow. These additional tests offer greater diagnostic accuracy, with active resistance tests showing likelihood ratios of 6.6 and 5.7 respectively[15]. This step-by-step approach aligns clinical evaluations with imaging results for a more precise diagnosis.
MRI plays a crucial role by identifying abnormalities that clinical tests might miss. For example, 31% of patients with gluteal tendinopathy showed MRI evidence despite negative clinical findings[5][6][7][15]. This highlights the value of combining multiple diagnostic tools since no single test can catch every case.
It’s also essential to consider patient-specific factors. For example, gluteal tendinopathy is more common in women over 40, so tailoring diagnostic strategies to patient demographics can improve accuracy[2][17][18]. By blending sensitive screening methods, targeted diagnostic tests, and patient-centered approaches, clinicians can develop a reliable strategy for accurate diagnosis and better outcomes.
FAQs
What is the most accurate clinical test to diagnose gluteal tendinopathy in patients with lateral hip pain?
One of the most reliable ways to diagnose gluteal tendinopathy is the single-leg stance test. During this test, if a patient feels lateral hip pain within 30 seconds of standing on one leg, it strongly indicates gluteal tendinopathy. The test boasts an impressive 98% diagnostic accuracy and 100% specificity.
This straightforward and non-invasive method provides healthcare professionals with a dependable way to confirm the condition and determine the appropriate course of treatment.
Why is it helpful to use multiple tests to diagnose gluteal tendinopathy?
Using several clinical tests can significantly improve the precision of diagnosing gluteal tendinopathy, especially in individuals experiencing pain on the side of the hip. This approach not only validates findings but also minimizes the risk of misdiagnosis, making it easier to pinpoint the condition with greater reliability.
By integrating multiple tests, healthcare providers can cross-reference results, boosting their confidence in the diagnosis. This, in turn, paves the way for more effective treatment plans and improved care for patients.
What does the specificity of the Single Leg Stance Test tell us about its accuracy in diagnosing gluteal tendinopathy?
The Single Leg Stance Test boasts a specificity of 100%, making it highly dependable for confirming gluteal tendinopathy when the result is positive. However, its sensitivity is quite low (38%), which means a negative result isn’t very effective at ruling out the condition.
In real-world clinical settings, this test works best when paired with other assessments to provide a more accurate diagnosis and enhance patient care.
Related Blog Posts
- Why Is Fatty Infiltration in the Multifidi Muscle Important for a Chronic Low Back Pain Prognosis?
- Dry needling versus cortisone injection in the treatment of greater trochanteric pain syndrome: A noninferiority randomized clinical trial
- What is the bursae denialist camp, and why is it important in relation to biomechanics and pain management?
- Tendinopathy: The Interplay between Mechanical Stress, Inflammation, and Vascularity



Comments are closed